All you need to know about black fungus infection -COVID 19
Whereas the second dysfunction of the COVID-19 pandemic is in the hands of India, Delhi doctors have reported a fungal disease caused by coronavirus infection. Since late last year in quite a few cities including Mumbai and Ahmedabad, cases of Mucormycosis or Black Fungus have already been tracked. In December 2020 and again this week doctors have expressed concerns regarding the increase in such cases, as there are up to 12 cases within 15 days. Dr. Manish Munjal, a senior ENT surgeon at Sir Ganga Ram Hospital, said these cases are registered with the patients of COVID-19.
WHAT EXACTLY THE BLACK FUNGAL INFECTION IS?
The new concern for medical professionals in some cities was the black fungus or mucormycosis. It also had caused death in transplantations and in intensive care (ICU) and in people with immunodeficiencies in the past. However, the rare disease recently recorded a rise in the number of patients recovering from COVID-19.
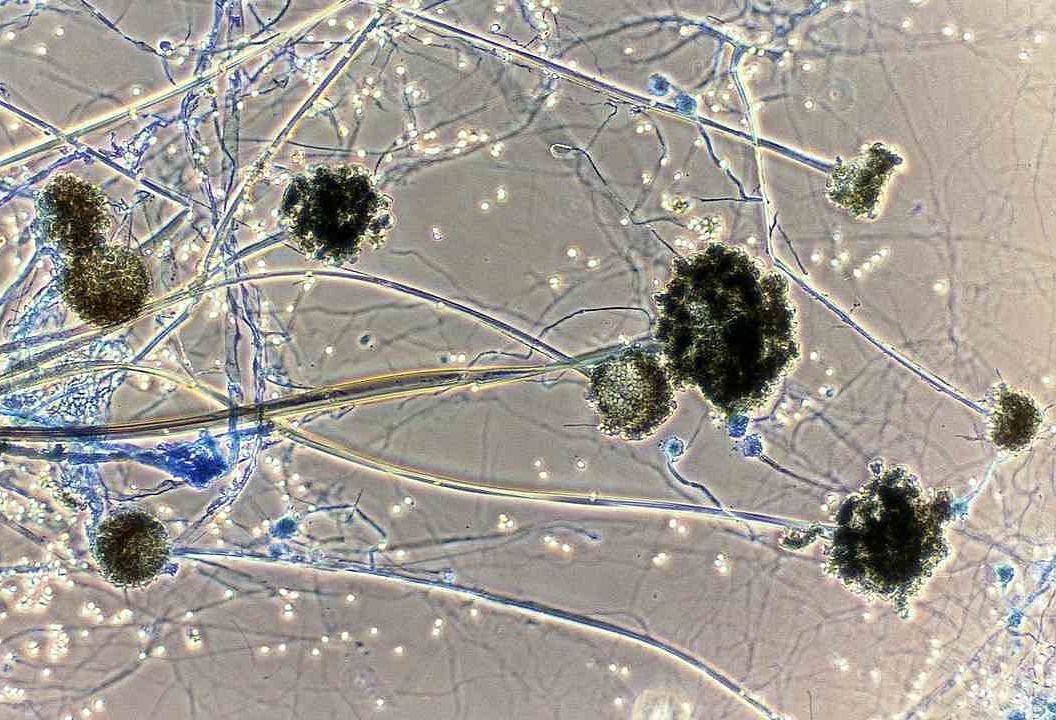
Mucormycosis is “serious but rare” and is caused by a group of molds, called mucormycetes, in the US Centers on Disease Control and Prevention. In most cases, the disease affects individuals who have previous health problems or take medications that decrease their capacity to deal with germs and diseases and are mainly caused by inhaling fungal air spores.
HERE ARE SOME SYMPTOMS OF MUCORMYCOSIS
Mucormycosis symptoms depend on where the fungus grows in the body and primarily affects any part of the body.
- One-sided face inflammation
- Congestion of the nose or sinus
- Black lesions on the nasal bridge of the mouth are becoming increasingly severe.
- Fever
- Headache
Pulmonary Mucormycosis Entailed
- Fever
- Cough
- Shortness of breath
- Chest pain
Besides, blisters or ulcers and the infected area can turn dark by Cutaneous (skin) mucormycosis. Pain, warmth, swelling, and excessive redness around the wound also include additional symptoms. In the gastrointestinal area, the pathogen results in abdominal pain, nausea, and vomiting, gastrointestinal bleeding.
How mucormycosis can be treated?
According to the US CDC, “Mucormycosis is severe and should be prescribed antifungal, usually amphotericin B, posaconazole or isavuconazole. Mucormycosis almost always requires surgery to cut off the tissue infected”.

